Overview
Cervical cancer happens when normal cells in the cervix change into abnormal cells and grow out of control. Most women whose cervical cancer is found and treated early do very well. If you’re in Ahmedabad and seeking care, finding a reputable cervical cancer hospital in Ahmedabad is crucial. The cervix is the bottom part, or neck, of the uterus.

FAQ's about Cervical cancer
Cervical cancer might not cause any symptoms at first. When it does cause symptoms, it can cause vaginal bleeding that occurs:
- In between menstrual cycles (meaning the bleeding happens when a woman is not having her period)
- After sex
- After menopause
These symptoms can also be caused by conditions that are not cancer. But if you have vaginal bleeding at these times, tell your doctor.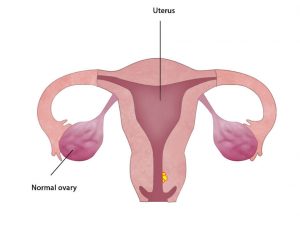
Pap Smear
A Pap test (also called a “Pap smear”) is used to screen women for cervical cancer.. Depending on your age, the doctor will also do a test for a virus called “human papillomavirus (HPV). Recurrent infection with HPV can cause cervical cancer.
If the test results are abnormal, the doctor will follow up with a test called Colposcopy and if required, a biopsy.
Colposcopy is direct microscopic examination by gynec oncologist to define the area on cervix responsible for shedding the abnormal cells. It is done after washing the cervix with saline and 1% acetic acid. The gynaec oncologist can see vascular as well as cellular changes through this examination and can define the abnormal area precisely. This abnormal area can be biopsied to confirm the grade of abnormality.
Biopsy
During a biopsy, the doctor will remove a tiny piece of abnormal-looking tissue from the cervix.
Doctors sometimes find cells in the cervix that are not cancer, but are abnormal and have a high chance of turning into cancer. If you have these “precancer” cells, your doctor can treat them in different ways.
Imaging
MRI pelvis with scanning of Upper abdomen and X ray chest. This will confirm the local extent of the disease and involvement of surrounding organs and lymph nodes.
Precancer conditions
CIN I (Early precursor lesion) – treatment options
- Observation and repeat smear after 6 months
- Cryosurgery or cauterization of abnormal area
- Laser Evaporation of lesion
CIN II and III (Definite precursor lesion for cervical cancer) – treatment options
- Conization – Cold knife conization / Laser conization/ LEEP
- Hysterectomy – if the patient has completed her child bearing
Cancer staging
Cancer staging is a way in which doctors find out how far a cancer has spread by clinical examination and investigations.
Clinical examination/ Examination under Anesthesia will involve per speculum, per vaginal and per rectal examination, which will give the gynec oncologist and idea about the size of the growth, involvement of surrounding tissues and the vaginal extension.
The right treatment for you will depend a lot on the stage of your cancer, your age, and other health problems. Your treatment will also depend on whether you might want to get pregnant in the future.
Cervical cancer can be treated in different ways.
Early disease (IA, IB, IIA) – In this the disease is limited to cervix or upper vagina. These warrant surgical treatment.
Locally Advanced disease (IIB, IIIA, IIIB) – In this the disease has extended beyond to involve the surrounding structures. This requires chemotherapy and radiotherapy primarily.
In certain cases when there is residual or recurrent disease, extensive surgery is required i.e. Pelvic Exenteration.
Locally Advanced disease (IV A) without nodal and parametrial involvement – This can be treated by extensive surgery i.e. pelvic Exenteration.
Metastatic disease – This is managed by chemotherapy.
- Surgery –
- Radical Hysterectomy Removing the uterus with cervix and upper part of the vagina along with removal bilateral parametrial and paravaginal tissues. Besides this, we also have to dissect the pelvic lymph nodes which are present on the great vessels of the lower limb on both sides – This is called a “radical hysterectomy” or Wertheim Meig surgery.
This can be done using Open/ Laparoscopic or Robotic techniques.
In Robotic Radical Hysterectomy, whole surgery is completed through 5 small holes. This is a Minimally Invasive Surgery, in which Radical Hysterectomy is done with robotic Assistance. It helps in early recovery and minimal blood loss. Fore more information, read Robotic surgery.
- Fertility Sparing Surgery – In patients who have not completed their family, fertility sparing surgery can be advised. This includes
- Conization – The cervical tumour along with the entire Transformation zone (cells of this area have the potential to become cancerous) is removed. The uterus and ovary are intact and patient can conceive.
- Radical Trachelectomy – Removing all or part of the cervix but leaving the uterus in place. The patient can bear the child as the uterus as well as the ovaries are preserved.
- Pelvic Exenteration – This is an extensive surgery, which may be required for advanced cases or patients having residual or recurrent disease.
- Anterior Exenteration – This surgery includes removal of urinary bladder in addition to Radical Hysterectomy. Then urine can be diverted bringing out a loop of bowel in which ureters are implanted. This is known as ileal conduit.
- Posterior Exenteration – This surgery includes removal of rectum in addition to Radical Hysterectomy. The stool passage can be restored or it may require stoma permanently.
- Total Pelvic Exenteration – This includes removal of urinary bladder, rectum, uterus, cervix, vagina and all pelvic soft tissues.
What is the human papillomavirus (HPV) vaccine? — The HPV vaccine helps keep people from getting infected with a germ called “human papillomavirus,” or “HPV.”
Why should I get the HPV vaccine? — The HPV vaccine can help keep you from getting an HPV infection. Being infected with HPV increases your risk of certain cancers:
- An HPV infection in the genitals can lead to cancer of the cervix (cervical cancer) or vagina (vaginal cancer) in women and cancer of the penis (penile cancer) in men. It can also cause genital warts in women and men.
- An HPV infection around the anus (anal cancer) can cause cancer of the anus in women and men.
- An HPV infection in the mouth and throat can lead to cancer of the mouth and throat in women and men.
How can people get infected with HPV? — People can get infected with HPV if their mouths or genitals touch the mouths or genitals of someone who is infected. People who have a lot of sex partners have a higher chance of getting an HPV infection.
What are the symptoms of an HPV infection? — Most people do not have any symptoms when they get infected with HPV. And often, the infection will get better on its own. But in some people, the infection doesn’t go away. People with a long-lasting HPV infection have a higher chance of getting cervical, vaginal, penile, or anal cancer, mouth or throat cancer, or genital warts. These problems usually happen many years after a person is first infected.
At what age do people get the HPV vaccine? — Most doctors recommend that people get the HPV vaccine at age 11 or 12. But people can get the vaccine any time from age 9 to 26. Women should not get the vaccine if they are pregnant.
What side effects can the HPV vaccine cause? — The HPV vaccine can cause redness, swelling, or soreness where the shot was given.
Does the HPV vaccine always work? — The HPV vaccine is very good at preventing HPV infection and cervical cancer. It might also prevent other cancers, including mouth and throat cancer. But it is not perfect. In some cases, people who get the vaccine can still get an HPV infection.
Do I need to be checked for cervical cancer if I get the vaccine? — Yes. All women, including those who get the HPV vaccine, should be checked on a routine schedule for cervical cancer. Most women are checked using a test called a “pap smear” starting at age 21.
What is a Pap test? — A Pap test (sometimes called a “Pap smear”) is a test that doctors use to check the cervix for early signs of cancer. The cervix is the part of a woman’s body where the uterus and the vagina meet. It is the bottom part of the uterus.
To do a Pap test, a speculum is inserted per vaginum and a tool is used to scrape cells from the cervix.
Pap tests can find cancer cells or cells that could turn into cancer, called “precancer.” Precancer can be treated to try to prevent cancer. The test can also usually find cancer in the early stages, when it can be treated or even cured.
When should a woman start having Pap tests? — Women should start having Pap tests when they turn 21. They do not need to be sexually active before they start getting Pap tests. When they turn 30, HPV test may be added.
How often should a woman have a Pap test? — That depends on how old she is and what the results of her past Pap tests have been.
- Women age 21 to 29 should have a Pap test every 3 years.
- Women age 30 and older can have a Pap test every 3 years or a Pap test and HPV test every 5 years.
- Women age 65 and older should stop having Pap tests if they meet all of these requirements:
- They have never smoked.
- They do not have a new sex partner since their last Pap test.
- They had Pap tests done regularly until they turned 65.
- They had 3 normal Pap tests in a row.
- They had no abnormal Pap tests in the past 10 years.
A woman might also get a Pap test if she has certain symptoms, such as vaginal bleeding.
Do I need to get Pap tests if I had a hysterectomy? — If you had surgery called a “hysterectomy” to remove your uterus, ask your doctor if you need to keep having Pap tests. If you no longer have a cervix, and if you did not have cervical cancer before your hysterectomy, you most likely do not need to have Pap testing after surgery.
Do I need to get Pap tests if I had the HPV vaccine? — Yes. HPV is the virus that causes cervical cancer. Getting the HPV vaccine reduces your chances of getting cervical cancer. But it does not completely protect you. You still need to be checked for cancer.
What if I have an abnormal Pap test? — First, you should know that abnormal Pap tests are common. They are just an initial test, and most women with an abnormal Pap test do not have cancer. If your Pap test has cells that look “abnormal,” your doctor or nurse can follow up with another test to find out for sure what is going on.
If it turns out that you have cervical cancer or precancer, there are effective treatments available. If your condition was found early, there is a good chance you can be cured.