Overview
Women have two ovaries, one on each side of the uterus. The ovaries, each about the size of an almond, produce eggs (ova) as well as the female sex hormones, oestrogen and progesterone. Ovarian cancer happens when normal cells in the ovary change into abnormal cells and grow out of control.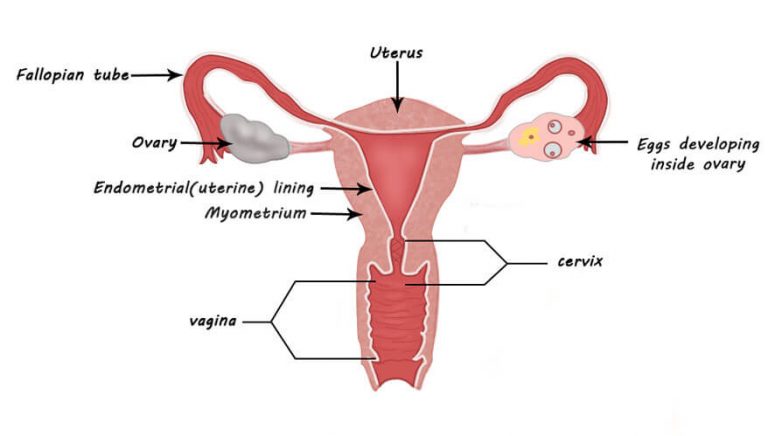
Female Genital Tract
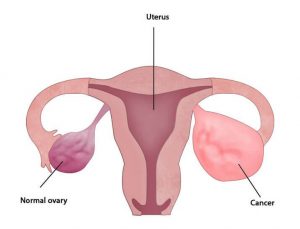
Ovarian Cancer
Ovarian cancer is the third most common cancer amongst women. It usually occurs in women above 50 years of age. It sometimes runs in families. Ovarian cancer often goes undetected until it has spread within the pelvis and abdomen. At this late stage, ovarian cancer is more difficult to treat. Early-stage ovarian cancer, in which the disease is confined to the ovary, is more likely to be treated successfully. Since the ovaries are located deep inside the abdomen, they are not easily accessible for examination. This along with vague symptoms make early detection of ovarian cancer a challenge.
The type of cell where the cancer begins determines the type of ovarian cancer which include:
- Epithelial tumours begin in the thin layer of tissue that covers the outside of the ovaries. About 90 percent of ovarian cancers are epithelial tumours
- Stromal tumours begin in the ovarian tissue that contains hormone-secreting cells. These tumours are usually diagnosed at an earlier stage than other ovarian tumours. About 7 percent of ovarian tumours are stromal.
- Germ cell tumours, which begin in the egg-producing cells. These rare ovarian cancers tend to occur in younger women.
FAQ's about Ovarian cancer
The symptoms of ovarian cancer are often not recognised early in the disease. They may also be so vague in the earlier stages, that they can easily be ignored. Some of the common symptoms are:
- Stomach ache and abdominal discomfort accompanied by a feeling of bloating or fullness of the stomach
- Abnormal vaginal bleeding
- Sudden weight gain or weight loss without any apparent reason
- Loss of appetite, nausea, vomiting, constipation and frequent urination in some cases
- Bloating
The exact cause of this disease is still under investigation. However, studies show those women are at higher risk who:
- Have no children
- Have had breast or colon cancer
- Use fertility drugs regularly
- Are on or have undergone hormone replacement therapy
Diagnosis of ovarian cancer starts with a physical examination, a blood test and a transvaginal ultrasound. The diagnosis must be confirmed with surgery to inspect the abdominal cavity, take biopsies and look for cancer cells in the abdominal fluid.
Ovarian cancer at its early stages is difficult to diagnose until it spreads and advances. This is because most symptoms are non-specific and thus of little use in diagnosis. The doctor may conduct vaginal or internal examination to investigate your ovaries and womb. They may also take a blood sample or refer you for an ultrasound scan.
The various methods used to diagnose ovarian cancer are:
Blood test (CA125)
The doctor may conduct a blood test to look for a chemical called CA125 in the blood. This chemical is produced by some ovarian cancer cells. A very high level of CA125 in the blood may mean you have ovarian cancer.
However, this chemical is not specific to ovarian cancer and may also be raised in many benign conditions, so a raised level of CA125 does not definitely mean you have ovarian cancer.
The National Institute for Health and Care Excellence (NICE) has produced guidance that advises your GP to test for CA125 if you frequently experience:
- Bloating
- Feeling full quickly
- Loss of appetite
- Pelvic or abdominal pain
The CA125 test is particularly important if you are 50 or over, or have these symptoms more than 12 times each month.
If in the test the patient has a raised CA125 level, then the doctor advices an ultrasound scan.
Ultrasound
An ultrasound uses high frequency sound waves to produce an image of the patient’s ovaries. An internal ultrasound also known as a transvaginal ultrasound is where the ultrasound probe is inserted into the vagina, or it may be an external ultrasound, where the probe is put next to the stomach. The image produced can show the size and texture of the ovaries, as well as any cysts that may be present.
Further tests
If the patient has been diagnosed with ovarian cancer, she will have to undergo further tests which will determine how large the cancer is and whether it has spread. This is called staging.
Further tests may include:
- Chest x-ray – this shows if the ovarian cancer has spread to the lungs or caused a build-up of fluid around the lungs
- CT scan or MRI scan – these imaging techniques are used to look for signs of cancer elsewhere in the abdomen and pelvis.
- Abdominal fluid aspiration – if there is a build-up of fluid in the abdomen and it looks swollen, it might mean that ovarian cancer has spread. To find out, a thin needle is passed into the abdomen to take a sample of fluid to be tested for cancer cells.
- Laparoscopy – this small operation may be performed if the gynaecologist wants to take a better look at the ovaries. A thin tube with a camera on the end is inserted through a small cut in the lower abdomen in order to examine your ovaries. A small sample of tissue may be taken from your ovaries for testing.
Depending on the stage of the ovarian cancer, the doctor recommends a customised treatment plan which is a combination of:
- Surgery
- Chemotherapy
Surgical treatment may be sufficient for malignant tumours that are well-differentiated and confined to the ovary. In addition, chemotherapy may be required for more aggressive tumours that are confined to the ovary. For patients with advanced disease, a combination of surgical reduction with a combination chemotherapy regimen is standard.
Surgery
Surgery is the preferred treatment and is frequently necessary to obtain a tissue specimen for differential diagnosis via its histology.
The type of surgery depends upon how widespread the cancer is when diagnosed as well as the presumed type and grade of cancer. The surgeon may remove one ovary and one fallopian tube if the cancer is localised in that ovary (stage one ovarian cancer). This may preserve the ability to become pregnant. If the cancer is in both ovaries and has not spread (stage two ovarian cancer), then both ovaries and fallopian tubes are removed, while the uterus is intact. This may still allow the patient to become pregnant by using frozen embryos or eggs or eggs from a donor. If the cancer has spread to the uterus (stage three ovarian cancer), then along with the ovary removal, the patient may also undergo hysterectomy to remove the uterus, surrounding lymph nodes and a fold of fatty abdominal tissue (omentum).
For more aggressive cases, where the disease has spread to other organs in the abdomen, Cytoreductive Surgery is done (CRS). Ovarian cancer usually spreads through surface to peritoneum that is the inner lining of the abdomen. In CRS all the sites where cancer is present is removed including the peritoneum. In some cases it is followed by HIPEC. For more imformation on HIPEC – read HIPEC.
Chemotherapy
Chemotherapy has been a general standard of care for ovarian cancer for decades, although with highly variable protocols. Mostly chemotherapy is given after surgery to prevent recurrence. The type and number of cycles depends on the pathology report i.e. the report after checking all the organs that were removed during surgery under microscope. In some cases, there may be reason to perform chemotherapy first, followed by surgery.
Targeted therapy
Targeted therapy uses medications that target the specific vulnerabilities present within the cancer cells. Targeted therapy drugs are usually reserved for treating recurring ovarian cancer after initial treatment and/or cancer that resists other treatments. The cancer cells are tested to determine which targeted therapy is most likely to be effective.
Targeted therapy is an active area of cancer research. Many clinical trials are testing new targeted therapies.
Radiation
Radiation therapy is not effective for advanced stages because when vital organs are in the radiation field, a high dose cannot be safely delivered. Radiation therapy is then commonly avoided as the vital organs may not be able to withstand the problems associated.